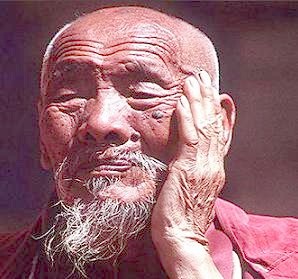
Pria Tua Berpeluang Menghasilkan Anak Cacat
Ketika bayi lahir menyandang cacat atau belakangan diketahui mengidap penyakit turunan tertentu, tuduhan biasanya dialamatkan ke sang ibu. Ini jamak. Apalagi jika ia sudah setengah baya. Sebaliknya, si bapak praktis terbebas dari gunjingan. Malah si bapak cenderung selalu dianggap subur, mampu menjadi bapak anak-anak sehat, bahkan sampai jauh memasuki usia senja.
Namun, belakangan, bukti-bukti makin bertumpuk bahwa pada lelakilah, bukannya wanita, yang kemungkinan menjadi sumber sebagian besar mutasi genetik baru.
|
|
Dan, karena itu, boleh jadi lelaki bertanggung jawab atas mayoritas penyakit-penyakit bawaan, yang sepintas tak jelas asal-usulnya. Pasalnya, kian tua pihak lelaki kian tinggi peluang spermanya mengalami mutasi genetik.
Pandangan baru ini sebagian besar bertumpu pada kajian-kajian mutakhir atas sel individual. Jadi, memang belum final. Masih banyak yang perlu dipelajari tentang mutasi genetik, demikian digarisbawahi sementara ilmuwan. Begitu pula, masih belum jelas benar seberapa besar variasi kecil dalam "cetak biru" genetik yang ada pada manusia nantinya akan "diterjemahkan" menjadi suatu cacat lahir.
Sering berbagi
Namun, yang pasti sebagian peneliti mengakui bahwa sekaranglah saatnya untuk lebih mengamati kemungkinan "kekeliruan" bawaan sel-sel sperma. Ini merupakan subyek yang selama ini tak begitu mendapat perhatian," kata Dr James Crow, ahli genetik di Universitas of Wisconsin, Madison, Amerika Serikat. Bidang ini memang belum lama dicermati.
Sekitar setengah abad silam, JBS Haldane, ahli genetik terkemuka Skotlandia, menduga bahwa kasus hemofili yang baru muncul di tengah keluarga yang sebelumnya tak mencatat sejarah penyakit demikian-agaknya merupakan hasil "pelesetan" genetik yang bersumber dari sperma lelaki, bukan sel telur wanita. Inu bukannya tanpa dasar. Para ilmuwan menyadari sepenuhnya bahwa kendati sel telur wanita telah terbentuk penuh selama pengembangan janin dan tak lagi mengalami pembagian sel lebih lanjut setelah lahir, sel kelamin "moyang" yang mencikal-bakali sperma lelaki akan terus berbagi sepanjang hidup seseorang. Dan, makin besar banyaknya pembagian sel, makin besar pula peluang minor error yang disebut mutasi titik bisa terjadi sewaktu kromosom tengah diduplikat. Malah belum lama ini, para ilmuwan berhasil memperlihatkan bahwa gen-gen pada kromosom Y yang cuma dimonopoli lelaki (karena berkromosom XY) ternyata memang bermutasi pada laju lebih cepat daripada gen-gen pada kromosom X, yang sebenarnya tak cuma dimiliki wanita (XX).
Berdasarkan ini, plus sejumlah kajian lain, para ilmuwan menaksir bahwa laju mutasi genetik keseluruhan dalam sel-sel sperma enam kali lebih tinggi daripada dalam sel telur. Dan, kesenjangan itu makin melebar seiring usia. Makin uzur lelaki, makin sering sel-sel "moyang" sperma berbagi, maka makin tinggi banyaknya kemungkinan mutasi titik yang barangkali tertumpuk dalam kromosom. Pada usia 13, tatkala seorang bocah laki-laki biasanya mulai memproduksi sperma, sel-sel kelaminnya itu telah berbagi sekitar 36 kali, dan berbagi sekitar 23 kali setahun sesudahnya. Pada umur 20, sel-sel sudah mengalami replikasi kira-kira 200 kali. Saat 30. kurang lebih 430 kali. Dan begitu menginjak 45, kira-kira 770 kali.
Statistik
Bukti statistik mendukung pula dugaan bahwa seorang pria yang menjadi bapak pada usia lebih tua, makin berpeluang menghasilkan anak penyandang cacat lahir daripada pria lebih belia, demikiar. diungkap Crow. Rata-rata, para bapak dari anak-anak yang mempunyai suatu penyakit genetik dominan, penyakit disebabkan satu cacat tunggal yang belum pernah terjadi sepanjang sejara.h keluarga sebelumnya, ternyata enam tahun lebih sepuh daripada bapak-bapak para anak yang tanpa penyakit. Misalnya, bapak lebih tua menghadapi peningkatan risiko memiliki anak dengan derita achondroplastic dwarfism, sindrom marsfan serta myositis ossificans.
Bagaimana dengan kaum hawa? Menjadi ibu pada usia lebih tua sebegitu jauh masih menghadapi peningkatan risiko melahirkan bayi dengan berbagai cacat lahir. Bedanya, bukan dikaitkan dengan mutasi titik, namun kesalahan replikasi seluruh kromosom. Contoh yang paling terkenal adalah triplikasi dari kromosom 21 yang menimbulkan sindrom Down.
Crow menambahkan, cacat kromosomal skala besar macam itu mudah dideteksi dalam tes prakelahiran. Jadi, masih terbuka kemungkinan diantisipasi. Sebaliknya, sebagian besar error genetik kecil-kecil yang diperkirakan sebagian besar dari pihak bapak, sampai sekarang susah didiagnosis secara dini sehingga baru ketahuan saat bayi dilahirkan. "Saya kira kita dapat sedikit mengeliminasi mutasi pada manusia jika kaum lelaki bereproduksi pada usia muda. Atau jika memang ingin punya anak belakangan, simpan saja spermanya yang masih muda dalam nitrogen;" sarannya.
DR AUDREY LUIZE
Alumnus Fakultas Kedokteran Universitas Airlangga Surabaya
Sumber : Kompas, 9 Mei 2003

|
Americans have excessively high blood cholesterol levels. The National Cholesterol Education Program (NCEP ATP III, 2001) states that a sound diet, weight loss and physical activity are the cornerstones of therapy for many individuals with cholesterol disorders. (Cholesterol-lowering drug therapy is reserved for those who have the very highest lipid levels or for those who have diabetes or coronary disease.) Atherosclerosis is a costly and fatal disease. Although there is no known cure, new evidence suggests that intensive lowering of serum total cholesterol, or more specifically, LDL cholesterol may retard the progression of coronary artery disease. The box, right, contains the NCEP cholesterol guidelines authored in 2001 by a panel of physicians and lipid experts. Reducing cholesterol through exercise, particularly LDL cholesterol, can be quite labor intensive. When individuals accumulate a sufficient weekly volume of exercise they can lower both total cholesterol and LDL-cholesterol and increase HDL-cholesterol (the “good” cholesterol). Exercise itself does not “burn off” cholesterol like it can with fat tissue. However, when exercise is of sufficient volume, for example, an adequate weekly frequency and duration, it can significantly reduce triglycerides and stimulate several metabolic enzyme systems in the muscles and liver to convert some of the cholesterol to a more favorable form, such as HDL-cholesterol. Reducing triglycerides decreases triglyceride-rich particles that are known to promote the growth of fatty deposits on artery walls. For many people with cholesterol disorders the first choice of therapy is dietary modification. In general, reducing high-glycemic carbohydrates reduces triglycerides, and reducing saturated and trans-fat foods decreases LDL-cholesterol. If LDL cholesterol (the “bad” cholesterol) is high enough, dietary therapy is often supplemented with cholesterol-lowering drug therapy. Exercise is of tremendous benefit when used in combination with either of these two forms of therapy. For those who maintain a frequent and sufficient level of exercise, it is possible that their physician will reduce their cholesterol-lowering medication and in some cases stop it altogether. Here are guidelines that outline a systematic approach for favorably altering cholesterol levels with regular exercise: • If you have a less-than-desirable cholesterol level, or your doctor has indicated you have a cholesterol disorder, have your physician establish your cardiovascular health status before engaging in a vigorous exercise program. Your physician may elect to perform additional blood tests (e.g., C-reactive protein) and/or a graded exercise test with an ECG (treadmill stress test) on you first. • Choose dynamic forms of exercise that tend to last at least 20 to 30 minutes and are performed at moderate intensities. Moderate exercise intensities would be an approximate effort of four to seven, on a scale of one to ten with ten being near maximal exercise. • In general, for exercise to significantly lower cholesterol levels, a relatively high volume of exercise is recommended (e.g. 1,500 kcal or more per week). In 12 to 16 weeks this volume of exercise can reduce total cholesterol by 10 to 20 percent. Fifteen hundred calories expended during exercise is equivalent to three to four hours per week for the average unfit person performing moderate-intensity walking, swimming, walk-jogging or cycling. This volume of weekly exercise is approximately the same volume of physical activity required to lose weight. As a result, fat weight loss tends to be associated with increases in HDL-cholesterol and reductions in total cholesterol and LDL-cholesterol levels, especially fat lost around the waist and abdomen. A sample program would be to start with walking 20 minutes per day, four days a week. Over six to eight weeks, graduate this program to one hour, six to seven days a week of walking over hilly (variable) terrain or walk-jogging over relatively flat ground. An alternative would be to walk 50 to 60 minutes three days a week and take an aerobics class three days a week and perhaps two to three sets of singles tennis on the seventh day. It is important to know that lower volumes of weekly exercise can still produce many other benefits, such as improved fitness and overall health, reduced blood pressure and increased psychological well-being. An ACE-certified Clinical Exercise Specialist can help you make the connection safely and effectively. A heart attack is a life-threatening event. Everyone should know the warning signs of a heart attack and how to get emergency help. Many people suffer permanent damage to their hearts or die because they do not get help immediately. Each year, more than a million persons in the United States have a heart attack, and about half (515,000) of them die. About one-half of those who die do so within 1 hour of the start of symptoms and before reaching the hospital. Both men and women have heart attacks. Emergency personnel can often stop arrhythmias with emergency cardiopulmonary resuscitation (CPR), defibrillation (electrical shock), and prompt advanced cardiac life support procedures. If care is sought soon enough, blood flow in the blocked artery can be restored in time to prevent permanent damage to the heart. Most people, however, do not seek medical care for 2 hours or more after symptoms begin. Many people wait 12 hours or longer. Symptoms and Diagnosis The warning signs and symptoms of a heart attack can include: Chest discomfort. Most heart attacks involve discomfort in the center of the chest that lasts for more than a few minutes or goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain. Heart attack pain can sometimes feel like indigestion or heartburn. Discomfort in other areas of the upper body. Pain, discomfort, or numbness can occur in one or both arms, the back, neck, jaw, or stomach. Shortness of breath. Difficulty in breathing often comes along with chest discomfort, but it may occur before chest discomfort. Other symptoms. Examples include breaking out in a cold sweat, having nausea and vomiting, or feeling light-headed or dizzy. Signs and symptoms vary from person to person. In fact, if you have a second heart attack, your symptoms may not be the same as for the first heart attack. Some people have no symptoms. This is called a "silent" heart attack. The symptoms of angina (chest pain) can be similar to the symptoms of a heart attack. If you have angina and notice a change or a worsening of your symptoms, talk with your doctor right away. Diagnosis of a heart attack may include the following tests: EKG (electrocardiogram). This test is used to measure the rate and regularity of your heartbeat. A 12-lead EKG is used in diagnosing a heart attack. Blood tests. When cells in the heart die, they release enzymes into the blood. These enzymes are called markers or biomarkers. Measuring the amount of these markers in the blood can show how much damage was done to your heart. These tests are often repeated at intervals to check for changes. The specific blood tests are: Troponin test. This test checks the troponin levels in the blood. This blood test is considered the most accurate to see if a heart attack has occurred and how much damage it did to the heart. CK or CK-MB test. These tests check for the amount of the different forms of creatine kinase in the blood. Myoglobin test. This test checks for the presence of myoglobin in the blood. Myoglobin is released when the heart or other muscle is injured. Nuclear heart scan. This test uses radioactive tracers (technetium or thallium) to outline heart chambers and major blood vessels leading to and from the heart. A nuclear heart scan shows any damage to your heart muscle. Cardiac catheterization. A thin, flexible tube (catheter) is passed through an artery in the groin (upper thigh) or arm to reach the coronary arteries. Your doctor can use the catheter to determine pressure and blood flow in the heart's chambers, collect blood samples from the heart, and examine the arteries of the heart by x ray. Coronary angiography. This test is usually performed along with cardiac catheterization. A dye that can be seen by using x ray is injected through the catheter into the coronary arteries. Your doctor can see the flow of blood through the heart and see where there are blockages. Causes Most heart attacks are caused by a blood clot that blocks one of the coronary arteries (the blood vessels that bring blood and oxygen to the heart muscle). When blood cannot reach part of your heart, that area starves for oxygen. If the blockage continues long enough, cells in the affected area die. Coronary artery disease (CAD) is the most common underlying cause of a heart attack. CAD is the hardening and narrowing of the coronary arteries by the buildup of plaque in the inside walls (atherosclerosis). Over time, plaque buildup in the coronary arteries can: Narrow the arteries so that less blood flows to the heart muscle Block completely the arteries and the flow of blood Cause blood clots to form and block the arteries A less common cause of heart attacks is a severe spasm (tightening) of the coronary artery that cuts off blood flow to the heart. These spasms can occur in persons with or without CAD. Artery spasm can sometimes be caused by: Taking certain drugs, such as cocaine Emotional stress Exposure to cold Cigarette smoking
|

